

The animated cartoon The Jetsons, set in a technologically advanced future, briefly showcases the youngest son Elroy video conferencing with his doctor.
That's right; in the 1960s, a TV show — known for its whimsical and elaborate inventions of what the future could look like — predicted the prevalence of telemedicine in consumers' lives.
Modern technology has indeed facilitated the widespread deployment and adoption of telemedicine in health care practices of all sizes, but telemedicine isn’t necessarily a modern-day innovation.
To put it simply, telemedicine is the delivery of clinical services through telecommunications. Telemedicine is an affordable, convenient way for medical patients to see their physicians. Time is saved, costs are reduced, engagement is nurtured and neither patients nor providers miss out on face-to-face interactions since webcams enable patients and providers to see each other in real time.
Today’s discourse surrounding telemedicine involves effective reimbursement policies, legal parameters, the development of meaningful patient-provider relationships and leveraging trendy technology such as smart devices, artificial intelligence and blockchain in health care.
Let’s take a closer look at telemedicine, its evolution over the years, its pros and cons, and the benefits that telemedicine and telehealth in general offer to health care practices.
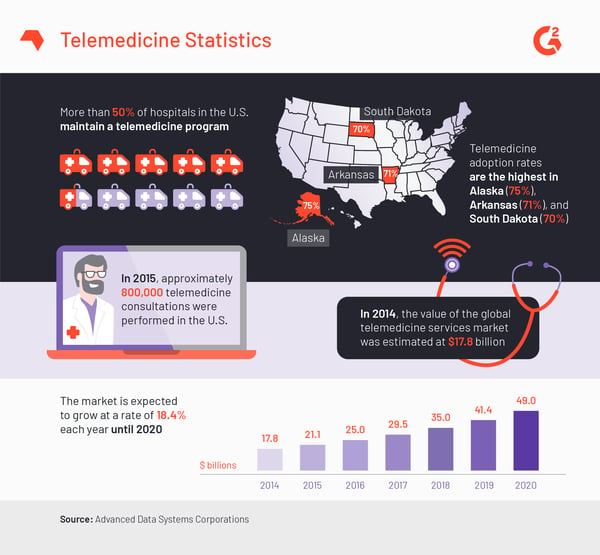
According to Advanced Data Systems Corporation’s comprehensive telemedicine description, here are several noteworthy telemedicine statistics:
Telemedicine has existed in some form since the 1950s, telemedicine company Chiron Health explains in their brief history of telemedicine blog post. Universities and hospital systems leveraged the telephone to share records, consultations and even patient images from one location to another. (A rather cool telemedicine concept was envisioned in 1925. Inventor Hugo Gernsback illustrated the “teledactyl,” a robot that offered a doctor video game-like controllers to remotely evaluate and diagnose their remote patient.)
 An illustration of the "teledactyl." Image courtesy of The Smithsonian.com
An illustration of the "teledactyl." Image courtesy of The Smithsonian.com
The goal was to connect with patients who resided in remote locations, delivering the same level of care as if that patient were in the same room as the medical professional. eVisit, creator of a telemedicine patient engagement platform, explained that in the 1960s, the US government funneled a lot of money into public health and defense departments to drive research and innovation in telemedicine.
While telemedicine still enables hospitals to deliver care to areas that are either remote or have scarce access to health care professionals and equipment, telemedicine has evolved to become more of a tool that offers convenience to even more patients.
This change has been spurred by developments in smart devices and personal medical devices. Patients are now empowered to track their own health on applications that live on their smartphones. Patients can even communicate with their primary doctors via HIPAA compliant messaging software, including texts and emails. Why should patients waste time in a waiting room when they can receive immediate care via video conference?
Because telemedicine continues to evolve, the distinction between telemedicine and telehealth is becoming less and less defined. In fact, the American Telemedicine Association (ATA) treats “telemedicine” and “telehealth” as interchangeable terms. After all, both telemedicine and telehealth provide patients and providers with the ability to participate in patient monitoring and consultation, to access medical information and expertise and even to transmit medical images and reports.
However, some vendors and users do like to differentiate the two.
In a nutshell, telehealth refers to the entire spectrum of remote health care services that are delivered via telecommunications and virtual technologies. Telemedicine is actually a way to provide clinical services through the medium of telehealth.
Telemedicine is a subset of telehealth, specifically the provision of clinical and medical services to patients through technology like video conferencing, text messaging, and audio. Telehealth is a broader concept than telemedicine, and can include services like patient monitoring via personal fitness tracking devices and non-clinical provider and administrative training.
There is also mHealth, which is shorthand for mobile health.
mHealth is a form of telemedicine that involves the provision of clinical and medical services through cell phones and other wireless, mobile devices. Examples of mHealth include: low-cost medical devices that can be attached to mobile phones or tablets, "smart" pill boxes that notify patients and caregivers should the patient forget to take their medication, and a variety of mobile health applications.
Without mHealth, telemedicine would be restricted to the Jetsons’ version of telemedicine: a video conferencing tool that provides virtual visits only.
mHealth takes advantage of the ubiquitous presence of cellphones and smart devices in consumers’ lives. Mobile health applications like Apple’s Health application and provider-supplied apps help the delivery of remote clinical care. Telemedicine has risen in popularity and usage because patients are taking advantage of the convenience factor. mHealth makes it possible for patients to take an active role in the self-management of their health.
There are three main classifications of telemedicine solutions that health care practices can leverage: remote patient monitoring (RPM), store-and-forward, and real-time.
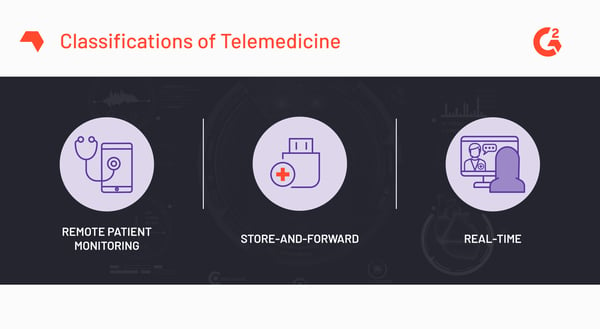
Remote patient monitoring (RPM), also referred to as telemonitoring, allows providers to track and monitor their patients with chronic diseases (diabetes, hypertension, etc.). RPM solutions equip remote caregivers with vital patient data such as blood sugar or blood pressure levels so that they can review such data in nearly real time and get notified if a measurement is abnormal. RPM solutions makes it possible for chronically ill, at-risk or recovery patients to stay at home instead of being confined to a hospital or clinic.
RPM solutions simulate in-person communication, so they depend on health tracking tools that accurately track patient health and efficiently send health data to the relevant health care professionals. RPM solutions provide incredible value to health care providers; with them, the number of readmissions falls, the ability to practice effective preventive care skyrockets and the physician-patient relationship flourishes.
Asynchronous telemedicine solutions, commonly referred to as store-and-forward telemedicine, enable providers to easily store and share patient medical data with other providers and practices. Asynchronous telemedicine solutions must therefore be secure, private and HIPAA compliant.
Asynchronous telemedicine solutions allow providers to experience the same kind of convenience that patients encounter with real-time telemedicine. Instead of relying on a bottlenecked process to share crucial patient data (during, for example, a referral), a primary doctor can leverage the technology to send an email with relevant information regarding a diagnosis for the ancillary care provider’s benefit.
Both clinical communication and patient outcomes are improved with asynchronous telemedicine. Patients, providers, technicians and physicians — all of these players can receive and access the same patient information, including lab results, X-rays or other clinical documentation, without needing to be in the same room at the same time.
Synchronous telemedicine exists as well. It is also known as real-time telehealth and it facilitates real-time communication between physician and patient. Generally, real-time telehealth solutions take the form of audio and video communication and replace in-person visits. Real-time telehealth can either be conducted in the comfort of the patient’s home or at a nearby medical facility. Synchronous telemedicine requires video conferencing or audio telecommunication platforms that are HIPAA compliant.
Notably, while synchronous telemedicine provides patients and physicians with an easy, convenient way to receive and provide medical treatment, health care providers have never intended it to fully replace in-person visits. Virtual telemedicine enables consultations, treatment recommendations and patient monitoring, but it’s intended to be an add-on service for people who have access to in-person medical treatment.
Specialty medical practices benefit from telemedicine as well. A variety of specialists find value in the ability to provide consultations via video or audio. Some of these include:
Patients undoubtedly benefit from telemedicine — just look at their expanded access to care via these solutions — but so do health care providers. Productivity, access to patient data and patient satisfaction can all be positively impacted when hospitals and clinics offer telemedicine. Additionally, the speed with which practices adopt telemedicine, and the success rates that those practices experience, has the ability to influence the rest of health care technology.
It must be noted that telemedicine has some limitations. Some of those limitations exist for a reason since telemedicine doesn’t aim to replace in-person patient-provider relationships entirely. Telemedicine aims to supplement and optimize the delivery of care, taking into consideration the high cost of health care and the growing pervasiveness of chronic diseases.
One area of telehealth and telemedicine that has huge untapped potential is chronic disease management. Chronic disease management can benefit if practices move away from supplemental care delivery and toward a fully integrated care model. Instead of an irregular check-in, add-on service, chronic disease management telemedicine can revamp the entire idea of preventive health care.
While providers can increase their availability beyond normal business hours, that doesn’t mean that the primary physician will be the one providing that after-hours service. However, when that happens, providers must deal with fragmented patient data. Fragmentation of patient data happens when providers must piece together a patient’s history from different sources. This can lead to results like inappropriate prescriptions and incomplete, unnecessary or redundant care.
Security is a significant concern with telemedicine. (Just take a look at this list of the top 10 biggest healthcare data breaches.) Health care data breaches are especially concerning because of the integration of key identity data (Social Security numbers, birth dates and employment histories, for example) and patient health data. Potential identity theft possibilities aside, hospitals and health care practices that run on outdated equipment and software, or that haven’t updated to the newest set of industry standards and regulations, open themselves up to severe consequences like errors in reimbursement, operating losses, wrong drug dosages and even harm to patients.
Sure, it’s good to take a look at the benefits a hospital or practice can receive from leveraging telemedicine technology, as well as the limitations they need to seriously consider. But you most likely want a quick run-down of the pros and cons of telemedicine, right?
Telehealth and telemedicine across all kinds of health care practices are natural evolutions of the medical industry thanks to technological advancements in telecommunications, mobile devices and online feedback. Health care is taking cues from other industries as the industry works double-time to keep up with ever-changing regulations and expectations in the delivery of care.
The technological innovations that impact and influence telemedicine correlate with changes in perspective in health care. Health care technological innovation help physicians and providers put patient satisfaction and engagement first, stress the importance of easy access to clinical services, and impress to vendors the benefit of affordable and easy-to-use health care software.
G2 recently created the much-needed telemedicine software category; please leave a review regarding the benefits and hurdles your practice experienced when adopting a telemedicine tool.
Jasmine is a former Senior Market Research Analyst at G2. Prior to G2, she worked in the nonprofit sector and contributed to a handful of online entertainment and pop culture publications.
 Diagnosis made easy
Diagnosis made easy
With increasing use of technology across all industries, using telemedicine software increase effective diagnosis.
Imagine you were feeling ill and could chat with your primary care doctor about your...
 by Jasmine Lee
by Jasmine Lee
In another sign of the growing telemedicine software market, healthcare practitioners continue...
 by Rachael Altman
by Rachael Altman
Last year, I predicted that patient engagement software would overtake telemedicine software...
 by Dominick Duda
by Dominick Duda


